Finding cancer’s fingerprint
In cancer, pathology plays a key role in determining treatment options. Using a microscope to examine cells and tissue collected from a biopsy, pathologists can identify what type of cancer a patient has and its stage. For decades, that was enough information for oncologists to predict the likely course of the disease and to plan treatment.
As science has advanced, however, cancer’s molecular make-up — DNA, RNA, proteins and other features — has become an increasingly important factor. It provides a fingerprint that offers additional clues to prognosis and which therapies will be most effective. This fingerprint, or mutational profile, can also serve as a marker for following the disease and its changes over time. It can be as important an indicator for beginning cancer treatment as it is for identifying remission and ending treatment.
The challenge is that scientists, pathologists and oncologists are still discovering mutations that drive cancer and therapies that will target them.

“No two cancers are the same,” explains Yi Ding, M.D., Ph.D., associate director of UR Medicine’s Molecular Genetic Pathology Unit. “Each delivers customized mutations that cannot be fully anticipated. It’s like a puzzle, and we’re trying to put all the pieces together.”
Ding and her team are keeping Wilmot Cancer Institute at this leading edge of precision medicine. Working closely with Wilmot’s clinicians, they are developing new tests to identify the genetic and molecular features of different cancers. Their work is essential to clarifying diagnosis and informing treatment plans, especially with complex cases. Not only can they help oncologists identify targeted therapies or clinical trials that address those features, they are also a starting point for monitoring minimal residual disease for clinical and research questions.
In the following conversation, Ding explains more about how molecular genetic pathology is changing the way we understand and treat cancer.
What can you learn from looking at a cancer’s mutational profile?
Quite a lot, actually. The cancer’s mutational profile is like its fingerprint, and we’re trying to find it as early as possible. It has implications for diagnosis, prognosis and treatment.
 For example, using tools called genomic sequencing assays, we can identify the genetic variations in all of a cancer’s cells. These variations can serve as indicators for which therapies might be most effective. This can be especially helpful for patients with metastatic cancer or cancer that does not respond to standard treatment. By looking at their mutational profile, we can identify features that make the patients eligible for clinical trials testing new targeted therapies.
For example, using tools called genomic sequencing assays, we can identify the genetic variations in all of a cancer’s cells. These variations can serve as indicators for which therapies might be most effective. This can be especially helpful for patients with metastatic cancer or cancer that does not respond to standard treatment. By looking at their mutational profile, we can identify features that make the patients eligible for clinical trials testing new targeted therapies.
These assays can also help us identify the tissue of origin for a cancer of unknown primary, a rare condition in which cancer cells are present in the body but the place where they began is not known. For some types of cancer, especially in their earlier stages, a patient may not need to be treated right away with targeted treatment and watchful waiting after management like surgery may be appropriate. In these cases, the mutations identified by molecular diagnostic assays serve as biomarkers that we can follow as we track the patient’s disease. Traditionally, we would track the patient by watching for clinical symptoms, but when they show up, it can be too late. This gives us an opportunity for early intervention.
Can you look at the molecular profiles of all cancers?
Like the Human Genome Project that was completed in 2003, a human cancer blueprint would be another incredible voyage of discovery. Because we don’t yet know the clinical significance of every mutation and because genomic sequencing is still very expensive, this kind of testing is not done for all cancers. Scientists and clinical investigators continue to study cancer’s genome, and eventually this kind of testing may become routine for every patient. For now, we focus on the gene variants that have the most impact on clinical care. We are trying to find targets we can act on — molecular features that make the cancer susceptible to specifically designed therapies. We are also looking for variants that predict sensitivity, resistance or toxicity to a specific therapy; that influence disease prognosis; or that serve as inclusion criteria for clinical trials.
With non small-cell lung cancer, for example, we look for molecular features such as mutations to the EGFR, KRAS, BRAF, ALK and ROS1 genes, or the presence of proteins such as PD1 or PD-L1. These genes and proteins are involved with mechanisms that encourage cancer’s growth, but they also have therapies specifically designed to target and interrupt them.
How do you see a cancer’s molecular features and how do you know what to look for?
We can’t actually look at a cancer’s molecular features the way we can look at cancer cells under a microscope. Instead, we take a very small sample of tissue from a biopsy and run it through a machine that does next-generation sequencing, or NGS.
Sequencing identifies the order of bases — called A, C, T and G, for short — in a strand of DNA. A next-generation sequencing machine can analyze the bases in millions of DNA strands simultaneously, and it gives us a report of every DNA sequence in the tissue.
This data can help us at an unprecedented level refine diagnosis and prognosis, and predict drug responses and the efficacy of treatments. It also enables us to evaluate disease susceptibility and monitor disease progression.
What if you don’t have a test available for the molecular feature you want to examine?
We work very closely with the oncologists at Wilmot Cancer Institute, and we are constantly working on expanding our test menu to meet clinical needs. If we don’t have a test they want, we develop one.
Since 2016, our lab has focused on NGS and the development of clinical applications. All of our clinical 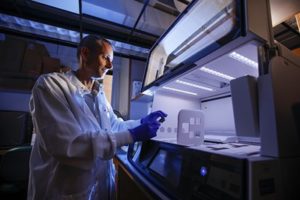 molecular diagnostic tests are laboratory-designed tests, meaning they are designed, manufactured and used within our laboratory. Our lab is Clinical Laboratory Improvement Amendments (CLIA) certified, and it is accredited by the New York state Department of Health and the College of American Pathologists.
molecular diagnostic tests are laboratory-designed tests, meaning they are designed, manufactured and used within our laboratory. Our lab is Clinical Laboratory Improvement Amendments (CLIA) certified, and it is accredited by the New York state Department of Health and the College of American Pathologists.
Recently, we developed a test for clonality — the first one designed and approved in New York state — which can help us figure out whether cancers in different parts of the body are derived from the same cells. This is especially helpful with lymphoma.
We recently had a case with a patient who, based on symptoms and a biopsy from the gastrointestinal tract, was diagnosed with mucosa-associated lymphoid tissue (MALT) lymphoma. The patient had also undergone a bone marrow biopsy as part of testing to determine the stage of the cancer. The bone marrow biopsy also showed evidence of lymphoma, and we needed to know whether it was related to the lymphoma in the GI tract. If it was related, that would have important implications for treatment planning.
Using our clonality test, we were able to confirm that they were unrelated lymphomas, and the patient’s treatment plans could remain the same. Tests like this are incredibly important in guiding how aggressive therapy should be and avoiding unnecessary treatment.
What are the biggest challenges in this field?
Molecular oncology is extremely complex, and we are still learning how to link molecular targets to cellular pathways involved in a cancer’s growth and survival.
There are also challenges associated with tumor heterogeneity and the potential limitations of a single biopsy. Tumor cells can have different profiles even within the same tumor, and different sites of metastases can have different tumor subclones and mutations.
Also, treating tumors with cytotoxic therapies such as chemotherapy before sequencing can often increase instability and alterations within a cancer’s genome, complicating our ability to determine tumor evolution and heterogeneity.
As more and more data come through genomic sequencing, there are other barriers for translating this into clinical practice, including cost-effectiveness and the ability to turn results around quickly.
How has this technology changed the role of pathologists in cancer?
Medicine has transformed at a dizzying pace over the last decade, much of it fueled by rapid advances in genomics and technology like NGS. As this technology becomes more widely available, pathologists will need to work more closely with clinicians to interpret and integrate these test results as part of an overall diagnostic work-up.
Understanding whether and how a gene plays a key role in the development of a cancer is important. For example, in lung cancer, adenocarcinoma (also called non-small cell lung cancer) and small cell lung cancer are biologically distinct. They both, however, can have a mutation of the EGFR gene. That mutation can make the lung adenocarcinoma more sensitive to a targeted therapy, but it may not have such benefit in the small cell lung cancer, in which further study of the genetic characteristics of such mutations is still needed.
Similarly, a mutation of the BRAF V600E gene may predict sensitivity to a targeted therapy called a monoclonal antibody for melanoma. In contrast, that same mutation negates the benefit of that monoclonal antibody in colorectal cancers that have wild-type KRAS mutations.
Furthermore, the presence of a mutation or other ayptical molecular results may not necessarily be an indicator of malignancy.
The complexity is amazing. In the molecular era, pathologists will be critical in guiding clinicians on how to interpret molecular findings, and together, they will be central to the effort of precision medicine.
December 2017