Research shows exercise a boon for cancer patients

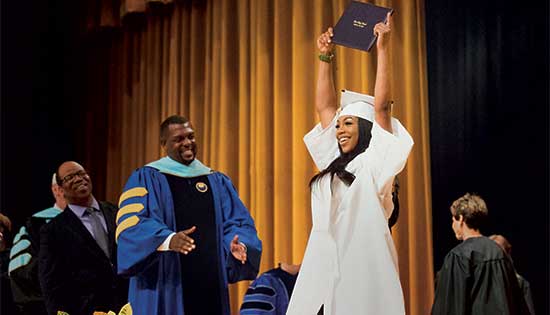
Karen Mustian, Ph.D., M.P.H.
Exercise and/or psychological therapy work better than medications to reduce cancer-related fatigue and should be recommended first to patients, according to a Wilmot Cancer Institute-led study published in JAMA Oncology.
“If a cancer patient is having trouble with fatigue, rather than looking for extra cups of coffee, a nap, or a pharmaceutical solution, consider a 15-minute walk,” said lead author Karen Mustian, Ph.D., M.P.H., associate professor in the University of Rochester Medical Center Department of Surgery’s Cancer Control Program. “It’s a really simple concept but it’s very hard for patients and the medical community to wrap their heads around it because these interventions have not been front-and-center in the past,” she added. “Our research gives clinicians a valuable asset to alleviate cancer-related fatigue.”
Scientists reached their conclusions about exercise and psychological interventions after analyzing the outcomes of 113 unique studies that tested various treatments for cancer-related fatigue. All were randomized clinical trials, the gold standard for evaluating effective treatments. The analysis started with 17,033 abstracts and was whittled down to 113 that met strict criteria of rigorous scientific methods.

More than 11,000 patients were involved in the 113 studies. Nearly half were women with breast cancer; ten studies focused on other types of cancer and enrolled only men.
Data show that exercise alone—whether aerobic or anaerobic—reduced cancer-related fatigue most significantly. Psychological interventions, such as therapy designed to provide education, change personal behavior, and adapt the way a person thinks about his or her circumstances, similarly improved fatigue. Studies that delivered a combination of exercise and psychological therapy had mixed results and researchers cannot say for sure what the best method is for combining treatments to make them effective. Finally, the study showed that drugs tested for treating cancer-related fatigue were not as effective. (Those drugs include stimulants like modafinil, which can be used for narcolepsy, and Ritalin, which treats ADHD.)
“The literature bears out that these drugs don’t work very well although they are continually prescribed,” Mustian said. “Cancer patients already take a lot of medications and they all come with risks and side effects. So any time you can subtract a pharmaceutical from the picture it usually benefits patients.”
All of the participants in the analyzed studies suffered cancer-related fatigue, the most common side effect during and after cancer treatment. This type of fatigue is different from being chronically tired, Mustian said. It’s a crushing sensation that’s not relieved by rest or sleep, and can persist for months or years. Researchers believe cancer-related fatigue might be the result of a chronic state of inflammation induced by the disease or its treatment. Most concerning, Mustian said, is that fatigue can decrease a patient’s chances of survival because it lessens the likelihood of completing medical treatments. She noted that the National Cancer Institute has chosen cancer-related fatigue as a top research priority.
Mustian and several colleagues at Wilmot have been studying exercise in the context of cancer for nearly 15 years. Her studies often test gentle yoga, walking, resistance bands, and other forms of movement as therapies to abate side effects. The Wilmot team also investigates the biological pathways impacted by exercise in cancer patients.
Co-authors of the current study include several members of Wilmot’s Cancer Control group, as well as national experts from the Society of Behavioral Medicine’s evidenced-based behavioral medicine committee. The NCI funded the research.
—Leslie Orr, March 2017